Bladder pain syndrome can cause pelvic pain and is often accompanied by urinary symptoms.
Bladder pain syndrome affects the bladder wall, the structure that stores and releases urine.
One possible cause involves changes in the protective layer of the bladder lining, allowing irritating substances to penetrate.
Learn more about this condition.
What is Bladder Pain Syndrome (Interstitial Cystitis)?
Bladder pain syndrome, also known as interstitial cystitis, is inflammation of the bladder. It is considered chronic pelvic pain because it is recurrent and lasts longer than 6 months.
Its symptoms can resemble a urinary tract infection, such as burning when urinating, urgency, and increased urinary frequency.
Bladder infections are usually related to bacteria; bladder pain syndrome, however, is generally not caused by a bacterial infection and may involve different mechanisms (such as changes in the mucosa and nerve sensitization).
Symptoms of Bladder Pain Syndrome
Most common urinary signs
The most common symptoms of bladder pain syndrome include the urinary changes below.
- Persistent urinary urgency: a sudden and intense need to urinate, often with a small urine volume.
- Pain, burning, and pressure in the bladder: which can also involve the urethra and the entire pelvic region.
- Increased urinary frequency: needing to urinate many times throughout the day and night.
Related: Pain when urinating: Causes and what to do
Symptoms that worsen during flare-ups
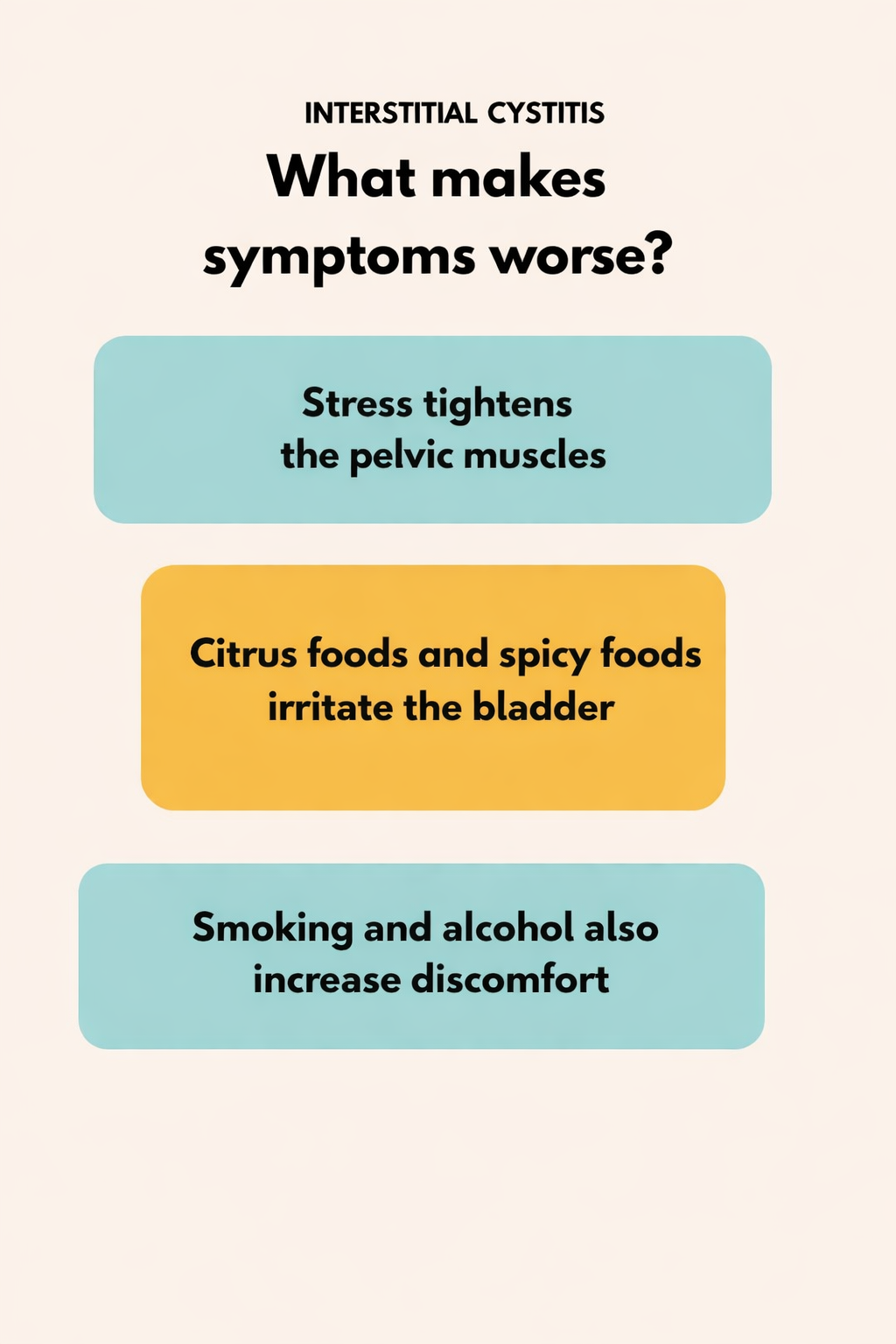
Bladder pain syndrome symptoms often worsen in certain situations.
Stress, for example, can intensify pain when urinating because it tenses muscles and amplifies existing discomfort.
Even your diet can play a role. Citrus fruits, tomatoes, chocolate, and spicy foods may worsen interstitial cystitis.
For some people, these items increase sensitivity and make discomfort worse. Smoking and alcoholic beverages may worsen symptoms in some patients.
What causes bladder pain syndrome?
The causes of interstitial cystitis are not fully known, but some hypotheses may help explain it.
- Changes in the layer that lines the bladder.
- Immune dysfunction that triggers an exaggerated inflammatory response.
- Involvement of pelvic nerves.
How is interstitial cystitis diagnosed?
The evaluation usually includes tests to rule out other causes and support the diagnosis, such as:
- Urine tests to rule out the presence of bacteria.
- Cystoscopy, an examination of the bladder using a thin tube with a camera.
- Urodynamic testing to assess how the bladder and urethra function.
How does bladder pain syndrome affect daily life?
The condition can impact different areas of quality of life, depending on symptom intensity and how often symptoms occur.
- Affects sleep: urinary urgency can interrupt sleep and cause daytime fatigue.
- Reduces productivity: frequent bathroom trips can disrupt work and study.
- Limits physical activity: high-impact exercise, such as deep squats and running, can put pressure on the pelvis and may worsen symptoms.
- Impacts sex life: persistent pain from bladder pain syndrome can make intimacy more difficult, especially during flare-ups.
- Affects mental health: symptoms can increase anxiety and lead to social withdrawal. For this reason, it may be helpful to combine urologic care with psychological support.

How to treat Bladder Pain Syndrome (Interstitial Cystitis)
Treatment for bladder pain syndrome varies by severity and can include several measures:
- Medications: pain relievers, antihistamines to reduce irritation, or antidepressants (in some cases), with the goal of modulating pain and symptoms, depending on medical evaluation.
- Pelvic floor physical therapy: to strengthen pelvic muscles;
- Bladder instillation: using a catheter to deliver medication into the bladder.
- Diet changes: reducing, as much as possible, foods that may worsen interstitial cystitis, such as citrus fruits, spicy foods, chocolate, and caffeine.
- Hydration:to support urinary comfort and help avoid symptom worsening, as advised.
Clinical management of bladder pain syndrome also includes lifestyle habits that support quality of life, such as stretching, light walks, and meditation to reduce stress.
When should you see a urologist?
It is recommended to see a urologist if you have symptoms such as:
- Persistent pain.
- Ongoing urinary urgency that affects daily life.
- Pain that disrupts or makes sexual activity difficult.
Frequently asked questions
What are the symptoms of bladder pain syndrome?
Pelvic pain and pressure, urgency, and increased urinary frequency.
What medication is used for bladder pain syndrome?
Treatment may include pain relievers, antihistamines, or antidepressants to help reduce pain, depending on medical evaluation.
Which emotion affects the bladder?
Stress can affect the bladder by increasing local muscle tension, contributing to an urgent need to urinate.
How can you tell if the pain is coming from the bladder?
If pain worsens when the bladder is full and improves after urinating, this may suggest bladder involvement — but an evaluation is needed to confirm.
Talk to Dr. Paulo Egydio
Bladder pain syndrome can affect work, relationships, and men’s self-esteem. With appropriate care, it is possible to improve quality of life.
Fill out the pre-assessment form to schedule a consultation with Dr. Paulo Egydio to discuss your symptoms.





